DAN medical information specialists and researchers answer your dive medicine questions.
I live inland near a lake that is 1,800 feet above sea level. Do I need to make special considerations when planning a dive there? Since I live at a similar altitude, am I acclimated and not required to make changes?
Many dives take place in inland lakes and rivers, some of which are at an altitude above sea level. When planning a dive, we need to consider two factors: The dive table and computer algorithms are based on being at sea level, which equals 1 atmosphere (atm), and are calculated for seawater, not fresh water. A dive at 2,000 feet above sea level will have a surface pressure of 0.93 atm. You will accumulate inert gas just as you would on any other dive, but when you surface the barometric pressure will be lower than at sea level. The standard dive tables are designed for a particular altitude range, usually at 1,000 feet mean sea level or less. A variety of tables will allow you to convert your dive planner of choice to reflect an altitude dive, and some tables are designed for altitude use.
Keep in mind that when ascending from a lower altitude to complete a dive at a higher altitude, you may need to treat your first dive as a repetitive dive. Many dive computers have a barometer or pressure sensor that samples the pressure when you turn them on at the dive site. A drawback to this feature is it senses the pressure of only where you are. The computer does not consider where you may have traveled from and may not account for the ascent. If your computer does not have a sensor, you will need to manually change the altitude settings. You will also need to set your computer for fresh water or salt water.
All dive-planning devices use mathematical calculations and theory. Always plan a conservative dive profile, dive well within the limits of your planning device, and allow for a safety stop. A diver should prepare for variances of diving in fresh water or at altitude and follow the rules of the planning device, regardless of the altitude where they live or to which they may have acclimated. The instruction guide provided with your dive table or computer will help you better understand their limits and help you enjoy happy and safe diving.
— Robert Soncini, NR-P, DMT
I suffered a hip fracture and three weeks ago had surgery to insert a plate and screws on the neck of my femur. Is it safe to dive eight weeks after surgery, and is there a risk of decompression illness (DCI) or osteonecrosis?
While you should seek a specific answer from a local physician trained in dive medicine, I can offer general guidelines. The industry standard for a return to diving after any fracture is for your doctor to release you for full and unrestricted activity, including contact sports, and then have an additional convalescent period of one-half the length of the regular healing time for the fracture. This extra time is to recover any lost physical fitness and aerobic capacity due to atrophy during the healing and rehabilitation process. If your doctor releases you for full and unrestricted activity after six weeks, for example, you should add three weeks for a total waiting period of nine weeks. These numbers are merely an example, and you should consult with your treating physician for a definitive answer.

The ability to conduct rigorous exercise, stress that joint through the range expected, and have a full recovery without restrictions, risk of injury, dislocation or other problems are issues to discuss with your surgeon.
Osteonecrosis is more closely related to long-term exposure without following the proper decompression protocols and is of very little concern in your case. There are very few documented cases of dysbaric osteonecrosis (DON) in recreational divers. Data suggest that scar tissue doesn’t ongas and offgas as efficiently as healthy tissue; however, diving well within recreational limits can mitigate, although not eliminate, risk of DCI.
— Lana P. Sorrell, MBA, EMT, DMT
I was diagnosed with ovarian cancer in June 2019 and received six chemo treatments. I was cancer-free by Nov. 15, 2019, but a scan revealed I had a pulmonary embolism. An ultrasound showed deep vein thrombosis (DVT) in my left calf and upper left arm and a third superficial DVT in my lower left arm. I have been on an anticoagulant since Nov. 17, 2019. When is it safe for me to dive again?
Dive medicine experts consider the use of a blood thinner to be a relative contraindication to diving. You can start to consider a safe return to diving after finishing the anticoagulant therapy. When both you and the treating physician understand and accept the risk involved, together you may make an informed decision whether to continue diving.
General risks are associated with diving while on anticoagulant medications. The greatest concern is the likelihood of severe bleeding and complications from even minor trauma such as ear or sinus barotrauma. There is also a theoretical risk of bleeding into the brain or spinal cord if decompression illness were to occur. Many dive physicians recommend using very conservative profiles to minimize this risk and making sure you can equalize your ears without difficulty if you decide to return to diving.
It is important to consider, especially if you travel to remote locations, that you are at an increased risk for bleeding. If you sustain an injury, there is no easy way to stop the bleeding, and many hospitals or clinics in remote locations do not have some of the products that can stop bleeding in extreme circumstances.
You should also discuss with your physician the reason for the anticoagulant prescription. Pulmonary embolisms and DVT have implications for fitness to dive independent of the issues associated with anticoagulant use. Your physician team will need to carefully assess the etiology of the DVT, location, associated medical conditions, resolution and the chance of its recurrence. A physician may find it reasonable to clear a patient for diving once the DVT has resolved and the risk of additional clots is low or well-managed and you have your condition regularly examined.
— Travis Ward, EMT-P, DMT
After the first week of a monthlong liveaboard trip I noticed the opening to my first stage was packed with a white powder. The divemaster suspected it was aluminum oxide from the tank. We cleaned the regulator and changed the tank, and I had to repeat this process a week later. The day after the second cleaning, my voice was hoarse, and my lungs felt irritated. I was concerned about the powder, but some other divers who were doctors thought that I had a cold and shouldn’t worry. When I got home, my lungs still felt irritated, and I had a cough and could hardly talk. An antibiotic helped a little, but my lungs soon felt much worse. Another doctor suspected asthma and prescribed prednisone and an inhaler, which I am still using often. I have a history of asthma but have had no issues in more than 20 years. Do you think it was aluminum oxide, and how dangerous is this for my lungs?
The white powder is most likely aluminum oxide. It is the result of corrosion inside aluminum cylinders. The visible white powder is about 50 microns (µm) in size. Most first-stage inlet filters have pore sizes of 5 µm, so the visible powder would be too large to pass through the filter, causing it to collect at the inlet filter of your first stage. Any particles smaller than that could pass through the filter to the second-stage regulator and into your breathing air. You may have breathed some finer particles of aluminum oxide.
You can open your second-stage regulator to see if any white powder has collected there. Although the human eye cannot see individual particles that small, enough accumulation may be visible. If many tanks of gas have been used with your regulator, it is impossible to know which tank was corroded.

Experts consistently agree that aluminum exposure is a serious concern. The position of the Department of Neurology and Psychiatry at Saint Louis University is that aluminum may cause liver toxicity and lead to degenerative symptoms, including Alzheimer’s.
There is no special treatment other than stopping the exposure if that is what caused your current respiratory condition and treating the respiratory condition itself. Unfortunately, there is no way to detect aluminum oxide in a tank other than opening the tank to inspect it. You can try to prevent your exposure by always using your own tanks. Scuba cylinders in the U.S. must have an annual visual inspection.
— Sheryl Shea, RN, CHT
I had an acoustic neuroma excision 20 years ago. As an active snorkeler I am well aware of barotrauma risks, and fortunately I have no problem equalizing my middle ear since the Eustachian tube is functional on that side. I am deaf in that ear, however, and understand the risk of hearing loss on my good side. Are there any dive-related risks besides hearing loss?
Acoustic neuromas are distinctive and usually benign growths of cells of the eighth cranial nerve. Essentially a brain tumor that develops within the adjacent structures of the brain, it grows into a round mass on the nerve where it emerges from the acoustic canal. Although some acoustic neuromas may produce noticeable symptoms, many are undetected until their growth begins to affect the brain stem and produce symptoms of partial or complete nerve deafness. Their advanced growth tends to affect the fifth and seventh cranial nerves and cause cerebellar ataxia and ultimately brain stem dysfunction. Fortunately, microsurgical techniques offer good results and can generally preserve the seventh cranial nerve and occasionally the patient’s hearing.
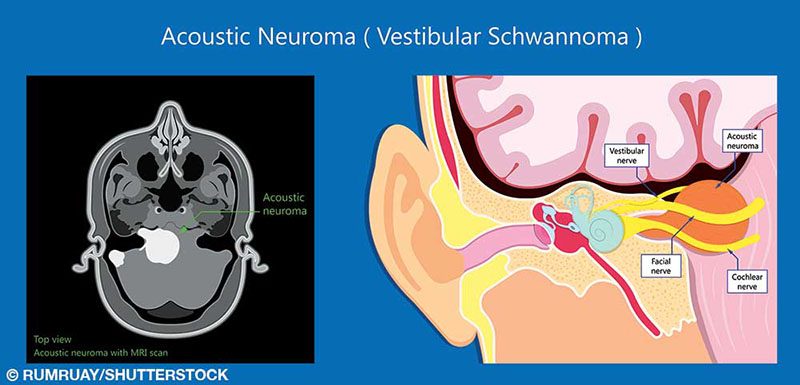
When considering diving, there are several issues to address: preexisting partial deafness and the risk of complete hearing loss due to barotrauma, physical or functional impairments that may interfere with the ability to respond to an emergency, and the difficulty for a physician to diagnose possible decompression illness. Patients are at risk for cerebrospinal fluid leaks, a relatively common complication that even without diving can produce symptoms of nausea and vomiting, neck stiffness and a sense of imbalance. In addition to unilateral hearing loss, they almost certainly cause disabling symptoms of unilateral vestibular loss (e.g., persistent dizziness, gait disturbances and imbalance). Additionally, temperature changes encountered during a dive (not necessarily thermoclines) may induce a caloric response of disabling vertigo as well as nausea and vomiting due to asymmetrical vestibular stimulation. In general, physicians trained in dive medicine recommend that patients avoid diving after acoustic neuroma surgery, regardless of the surgical approach.
— Daniel A. Nord, EMT-P, CHT
© Alert Diver — Q2 2020