Overview
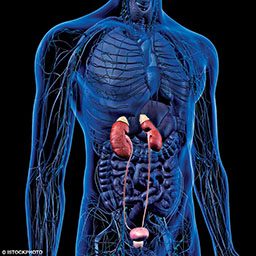
Dialysis is the common name for renal replacement therapy. This therapy is indicated when their kidneys suddenly stop working, or when there is a gradual decline in kidney function and people reach an end-stage renal disease (ESRD). Dialysis works through diffusion of solutes and ultrafiltration of blood through a series of semipermeable membranes. The therapy intends to take over the kidneys’ function, maintaining an adequate hydro-electrolyte balance and removing toxins and byproducts of metabolism. It can be a temporary measure while waiting for a kidney transplant or permanent when a transplant is not possible. But this technology cannot completely and effectively replace the kidneys, and patients undergoing dialysis often cope with a series of complications and side effects.
When a diver requires dialysis, they often ask their doctor about whether or not they can continue diving. This is answer is often not satisfactory enough, as diving physiology is often elusive for most doctors.
While each case is its own universe, below are some general concerns and considerations for people undergoing dialysis.
An individual’s medical and physical fitness to dive should always be addressed individually.
If you are currently seeking dialysis treatment, please take the time to share these general concerns and considerations with your doctor to make sure you can both make an informed decision on whether or not it is safe to continue scuba diving.
Overall Medical Fitness
Most people who end up with a stage of renal disease that requires dialysis are usually unable to meet many minimum requirements to mitigate the inherent risks of scuba diving. Patients with chronic kidney disease are usually on a number of medications, some of which may pose risks or contraindications to diving. The candidate should have no additional comorbidities that could increase the chances of a diving injury, or compromise the candidate’s health or safety.
Fluid Management
Patients on dialysis have a very delicate hydro-electrolyte balance. Diving causes some significant fluid shifts that impose a cardiovascular challenge. Under normal circumstances, these changes are usually well managed with a series of cardiovascular, pulmonary and renal responses. Unless you are diving in 100° F waters, immersion inevitably imposes a variable degree of heat loss. In an attempt to maintain our core temperature, the blood vessels in our skin undergo significant vasoconstriction. As a result, the volume of blood that usually flows through our skin is redirected to our core circulation. In addition, the increased hydrostatic pressure also mobilizes the extravascular fluid that normally pools in our lower extremities into central circulation. This fluid shifts from the skin, and lower extremities effectively increase the volume of circulating blood (hypervolemia) by up to 800 ml on an average-sized person. With the circulatory system being forced to deal with an excess of fluid, the cardiovascular system faces a challenge. Under normal circumstances, our body will manage this excess of fluid by increasing urine production, but a patient with chronic kidney disease will likely struggle to compensate via this method effectively. Failure to adequately manage this hypervolemic state could increase the risk of pulmonary edema and/or result in heart failure. Patients who can still produce urine should consider the cost of a forced and dramatically increased glomerular filtration.
Decompression Stress
Decompression stress is known to cause platelet and complement system activation. While this risk could be minimized by significantly limiting the overall exposure (depth, time, dive profile and ascent rates), it should still be considered a potential additional stressor.
Dialysis Access
Although hydrostatic pressure itself may not necessarily affect the dialysis access, consider the risk of any recreational physical activity disrupting the vascular access. Other considerations include a wetsuit being too tight on the access, which compromises flow and increases the risk of clotting. The effort in climbing up the ladder, combined the with the added weight of the water and BCD straps are also disruptors to vascular access. Consider also the risk of infections when exposed to natural unsanitized water.
Gas Narcosis
Elevated levels of byproducts of metabolism can cause a decreased level of alertness. This per se could be risky while diving. When added to the narcotic effect of gases like nitrogen and carbon dioxide, it is probably prudent to assume that the sum of all could have a synergic effect.
Exercise Tolerance
Anemia is commonly associated with renal failure. Hb levels should be normal to ensure the candidate can have adequate exercise tolerance and overall stamina, and normal blood pressure.
Access to Medical Care
Dialysis patients should take into consideration that diving usually takes place in areas where timely access to advanced medical intervention can not always be guaranteed.