DAN MEDICS AND RESEARCHERS ANSWER YOUR DIVE MEDICINE QUESTIONS.
© ISTOCK/ MPHILLIOS007
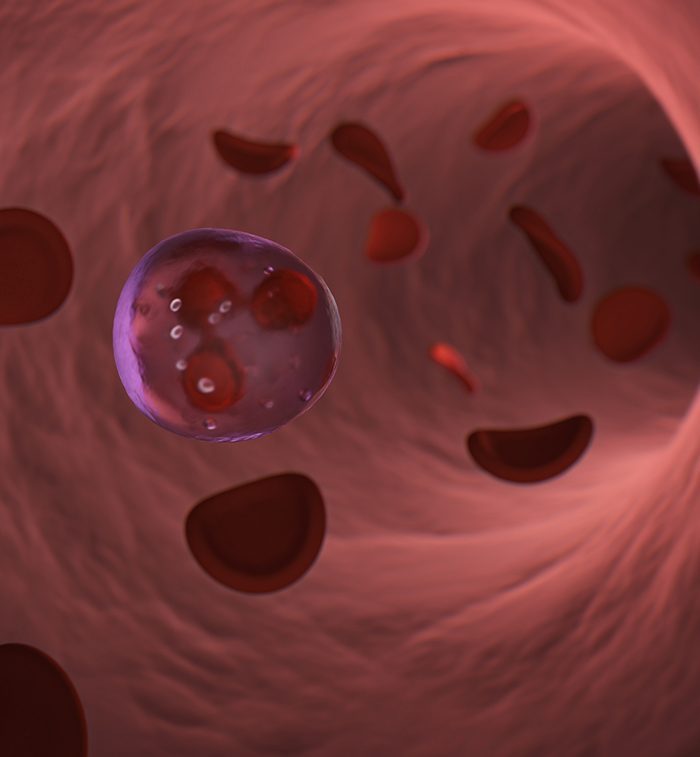
Q: I have been diagnosed with low platelets. Is it OK to dive?
Before you dive, you and your doctor should consider some possible effects of having a low platelet count. In some cases, it may affect the body’s ability to clot properly in response to injury. Cuts and bruises are common injuries in almost any recreational outdoor activity, so you should take extra care to avoid cuts and scrapes.
Middle-ear and sinus barotraumas are the most common dive injuries. They are typically self-limited, because normal coagulation stops the internal bleeding, giving divers time to seek professional medical treatment. When a diver has issues with clotting, pressure on the wound will control bleeding. Since pressure is not possible with internal bleeding, however, ordinary ear, nose, and throat barotraumas can become medical emergencies.
Decompression injuries add another dimension to bleeding risk, as bubble formation and growth cause microscopic tissue damage through mechanical tissue disruption and normal inflammatory processes. Coagulation can control these microbleeds, and recompression therapy can revert bubble growth, wash out inert gas, and minimize inflammation. When a diver has clotting issues, however, the microbleeding caused by bubbles can reduce the effectiveness of recompression therapy. This problem can be critical in severe cases, such as spinal cord involvement or an arterial gas embolism.
— Ben Strelnick, NREMT, W-EMT

© ISTOCK/WAVEBREAK MEDIA
Q: Six weeks ago I had a portion of my left lung’s lower lobe removed due to a nodule from stage 4 melanoma, and I am now starting immunotherapy. The surgeon and pulmonologist say it is safe to resume diving. Is there any specific information that suggests otherwise?
Diving is not recommended during any ongoing cancer treatment due to the unpredictability of the drugs used. You will likely be in poorer health and weaker than usual during treatment. Additionally, six weeks is insufficient for thorough healing after an invasive procedure. Complete recovery and a physician’s clearance for full and unrestricted physical activity are necessary before diving.
Generally, diving is not recommended after any surgery that removes a section of lung tissue. Changes in the lung’s structure can predispose you to a fatal pneumothorax. Since barotrauma can occur with lung tissue hyperinflation, the diver’s lungs must be able to tolerate rapid changes in volume and pressure.
Fibrotic or scarred tissue has reduced compliance, and any weakness in lung structure may rupture from even slight overinflation. Pneumothorax can be dangerous enough on its own, but the result may be fatal when it happens underwater. It can develop into a tension pneumothorax on ascent: The affected lung collapses, and the increased pressure underwater stresses the heart, vascular structures, and the healthy lung along with the heart and vascular structures.
We recommend that your care providers contact us directly for a consultation. AD
— Ben Strelnick, NREMT, W-EMT

This page is dedicated to the memory of Ben Strelnick (1984–2023), our DAN colleague and friend who passed away in May from a cave diving incident.
© Alert Diver — Q3 2023