Proceedings Summary | DAN/UHMS PFO and Fitness to Dive Workshop
Introduction
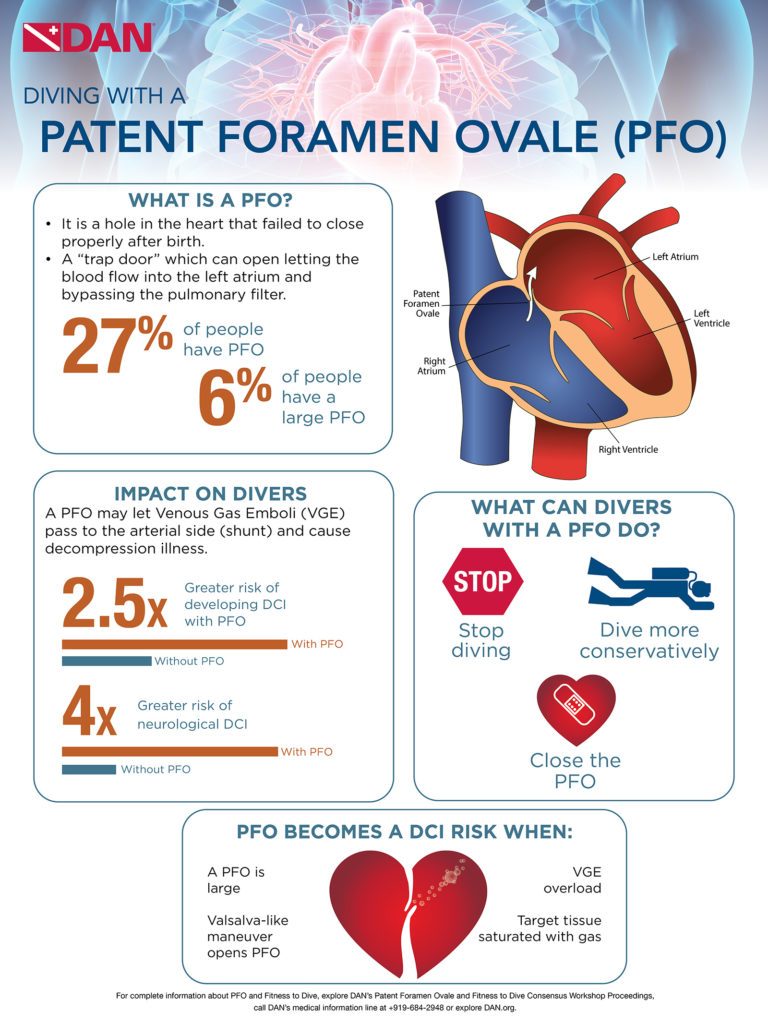
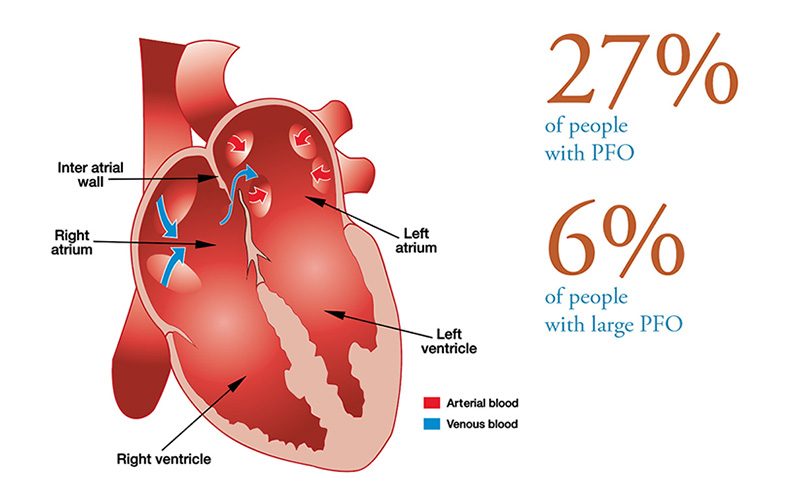
Prior to birth, oxygenated blood flows from the mother through the placenta to the heart of the fetus via the opening in the wall separating the left and right atrium (foramen ovale) into the fetal circulation. The foramen ovale has a “trap door” feature which opens due to the pressure of blood flow from the mother’s placenta entering the right atrium, and lets the blood pass to the left atrium. At birth, the lungs expand and the pressure in the left atrium increases and “slams shut” the foramen ovale. Shortly after birth the “door” fuses together, but in about 27 percent of people, it fails to fuse completely and results in a patent foramen ovale (PFO) also called persistent foramen ovale.
In people with PFO, if the pressure in the right atrium rises above the pressure in the left atrium, blood can flow from the right to the left atrium. The direct flow of blood from the right to the left atrium which bypasses the lungs is called right-to-left shunt (RLS). The RLS is known to let blood clots pass to the arterial side which can cause a stroke (brain trombo-embolism). Similarly, the PFO in divers may let gas bubbles from the venous blood — venous gas emboli (VGE) — pass the arterial side and cause decompression sickness.
Epidemiological studies have shown an association between PFO and certain types of neurological and cutaneous decompression sickness (DCS). The DCS risk in recreational divers has been reported at 3.6 cases per 10,000 dives, with 0.84 cases of neurological DCS per 10,000 dives and four-fold increase in risk with PFO. The overall risk of neurological DCS is low, even in the presence of a PFO. However, for some individuals, PFO seems to be a greater risk than predicted. Guidelines for PFO testing are aimed at identifying such individuals and managing their DCS risk.
The following guidelines were developed from the joint position statement on PFO and diving published by the South Pacific Underwater Medicine Society (SPUMS) the United Kingdom Sports Diving (UKSDMC), and the DAN sponsored workshop held in conjunction with the UHMS Annual Scientific Meeting in Montreal, Canada, June 2015.
Who Should Be Tested for PFO?
Routine screening for PFO at the time of dive medical fitness assessment (either initial or periodic) is not indicated. Consideration should be given to testing for PFO when there is a history of more than one episode of decompression sickness (DCS) with cerebral, spinal, vestibulocochlear or cutaneous manifestations.
Non-cutaneous manifestations of “mild DCI” as defined in the Remote DCI Workshop Proceedings [Consensus Statements, In: Management of Mild or Marginal Decompression Illness in Remote Locations, Workshop Proceedings (May 24-25, 2004). Mitchell SJ, Doolette DJ, Wachholz CJ, Vann RD, Eds. Divers Alert Network, Durham, NC, 2005, pp. 6-9.] are not indications for PFO investigation. Headache as an isolated symptom after diving is not an indication for PFO investigation.
PFO Testing and Evaluation Recommendations
PFO Testing
- Testing is undertaken by centers well practiced in the technique.
- The testing must include bubble contrast, ideally combined with trans-thoracic echocardiogram (TTE). Use of two-dimensional and color-flow echo cardiography without bubble contrast is not adequate.
- The testing must include the use of provocation maneuvers to promote right-to-left shunt including Valsalva release or sniffing as described in the supporting references (both undertaken when the right atrium is densely opacified by bubble contrast).
What Does a Positive Test Mean?
- A spontaneous shunt without provocation or a large, provoked shunt following diving when venous gas emboli are present is recognized as a risk factor for those forms of DCS with cerebral, spinal, vestibulocochlear or cutaneous manifestations.
- Smaller shunts are associated with a lower but poorly defined risk of DCS. The significance of minor degrees of shunting needs to be interpreted in the clinical setting that led to testing.
- Detection of a PFO after an episode of DCS does not guarantee that the PFO contributed to causation.
What Are the Options for Divers to Test Positive?
Following a diagnosis of PFO considered likely to be associated with increased DCS risk, the diver may consider the following options in consultation with a diving physician:
- Stop diving.
- Dive more conservatively. There are various strategies that might be employed to reduce the risk of significant venous bubble formation after diving, or the subsequent right-to-left shunting of such bubbles across a PFO. The appropriateness of this approach, and the strategies chosen, need to be considered on an individual basis, and in discussion with a diving medicine expert. Examples include: reducing dive times to well inside accepted no-stop limits; performing only one dive per day; use of nitrox with air dive planning tools; intentional lengthening of a safety stop or decompression time at shallow stops; avoidance of heavy exercise and unnecessary lifting or straining for at least three hours after diving.
- Close the PFO. It is emphasized, however, that closing a PFO after an episode of DCS cannot be considered to provide assurance that DCS will not occur again. The options outlined above require careful consideration of the risks and benefits and the clinical setting that led to screening.
When Can Divers Who Undergo Closure Return to Diving?
Following closure of a PFO and before returning to diving, the diver requires a repeat bubble contrast echocardiogram demonstrating shunt closure, a minimum of three months after the closure. Diving should not be resumed until satisfactory closure of the PFO is confirmed, and the diver has ceased potent antiplatelet medication (aspirin is acceptable).
CAUTION
Venous bubbles can also enter the systemic circulation through intrapulmonary shunts, although the role of this pathway in the pathogenesis of decompression sickness is not as well established as PFO. These shunts are normally closed at rest. They tend to open with exercise, hypoxia and beta adrenergic stimulation, and close with hyperoxia. It is therefore plausible that exercise, hypoxia and adrenergic stimulation after a dive could precipitate decompression sickness when it might not otherwise have occurred, while supplemental oxygen is likely to minimize this effect.
Facts About Divers With PFO
- Divers with PFO have 2.5 times greater overall risk of DCS than divers without a PFO and four times greater risk of neurological DCS. However, the absolute incidence of neurological DCS in divers with PFO is estimated at 4.7 DCS cases per 10,000 dives.
- A major study at the Mayo Clinic by Dr. Hagen and colleagues determined there is a large prevalence of PFO in young people, however it declines and levels off at approximately 27 percent. They also found that in each of the decade intervals, there is no difference in prevalence of PFOs between men and women.
- Four studies were compared, determining the prevalence of RLS or large PFO in divers with spinal DCI is 44 percent compared to 14.2 percent in controls, those without prevalence of RLS or large PFO.
- Half of the divers in the studies with RLS related DCI have a PFO that is a centimeter in diameter or larger, therefore the greatest risk of DCI is in those with the largest PFOs (six percent), not all divers with a PFO.
- Cerebral, spinal, cutaneous and inner ear DCS have been associated with PFO, however the link between PFO and cutaneous and inner ear DCS is the strongest. In approximately 74 percent of cases present with isolate inner ear symptoms (no other symptoms of hyperbaric related issues), 80 percent of the cases had a large spontaneously shunting PFO.
- There are factors necessary for PFO to contribute to DCS: you need to have a large PFO; venous gas emboli must form; bubble must cross the PFO (provocative factor to open PFO needed) to arterial circulation; and the bubbles must reach a target tissue while it is still supersaturated and vulnerable.
Denoble PJ, Holm JR, eds. Patent Foramen Ovale and Fitness to Dive Consensus Workshop Proceedings. Durham, NC, Divers Alert Network, 2015, 146 pp.
Patent Foramen Ovale (PFO) Infographic