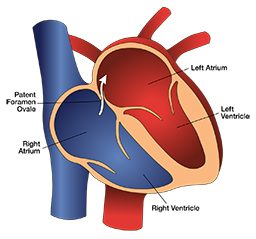
Patent foramen ovale (PFO) is a common congenital heart defect. It is a hole between the right and left sides of the heart. The foramen ovale is the wall separating the atria. Prior to birth, the foramen ovale has an opening that lets blood pass from the right to the left atrium. Shortly after birth this opening fuses. In about 27 percent of people, it fails to fuse completely.
With a patent foramen ovale, if the pressure in the right atrium rises above the pressure in the left atrium, blood can flow from the right to the left atrium (known as a right-to-left shunt or RLS). In divers, this may let gas bubbles from the venous blood (venous gas emboli or VGE) pass to the arterial side and cause decompression illness (DCI).
Patent Foramen Ovale and DCI Risk
Epidemiological studies show an association between PFO and certain types of neurological and cutaneous decompression illness (DCI). The risk of DCI is 2.5 times greater in divers with a PFO (and the risk of neurological DCI is 4 times greater).
The overall risk of neurological DCI is still low, even in a person with a PFO. For some people, PFO is riskier than predicted. The goals of guidelines for PFO testing are to identify such individuals and manage their DCI risk.
Testing for Patent Foramen Ovale
Routine screening for patent foramen ovale during a dive medical fitness assessment (either initial or periodic) is not necessary. You should have a PFO test if you have a history of more than one episode of DCI with cerebral, spinal, eighth cranial nerve or cutaneous manifestations.
Neither noncutaneous manifestations of mild DCI nor isolated headaches after diving are indications for PFO screening.
- The testing must include bubble contrast, ideally combined with a transthoracic echocardiogram (TTE). The use of two-dimensional and color-flow echocardiography without bubble contrast is not adequate.
- The testing must attempt to provoke right-to-left shunting, including Valsalva release or sniffing, while the right atrium is densely opaque with bubble contrast.
- A spontaneous shunt without provocation or a significant provoked right-to-left shunt with VGE following diving is a risk factor for DCI with cerebral, spinal, vestibulocochlear or cutaneous manifestations.
- Smaller shunts are associated with a lower but poorly defined risk of DCI. The significance of minor degrees of RLS needs evaluation in the clinical setting that led to testing.
- Detection of a PFO after an episode of DCI does not guarantee that the PFO contributed.
Positive PFO Test
Your diagnosis may be a PFO that is likely to increase DCI risk. If so, you can consider the following options in consultation with a diving physician:
- Stop diving.
- Dive more conservatively. Various strategies may reduce the risk of significant venous bubble formation after diving or the subsequent right-to-left shunting of bubbles across a PFO. It is best to discuss with a dive medicine expert the appropriateness of this approach and the strategies you can use. These strategies may include:
- Reducing dive times to well inside accepted no-decompression limits
- Doing only one dive per day
- Planning for air dives but breathing nitrox (while abiding by the actual gas’s maximum operating depth)
- Lengthening a safety stop or your decompression time at shallow stops
- Avoiding heavy exercise and unnecessary lifting or straining for at least three hours after diving
- Close the PFO. Closing a PFO after an episode of DCI does not ensure that DCI will not occur again. All of the options require careful consideration of the risks and benefits and the clinical setting that led to screening.
Return to Diving After Closure
Following the closure of a PFO and before returning to diving, you should have a repeat bubble-contrast echocardiogram. This test should demonstrate shunt closure at a minimum of three months after the surgery. You should only resume diving once a test confirms closure of your PFO and you are no longer taking potent antiplatelet medication.
Note: Venous bubbles can also enter systemic circulation through intrapulmonary shunts, although the role of this pathway in DCI is less well understood than that of a PFO. These shunts are typically closed at rest. They tend to open with exercise, hypoxia and beta-adrenergic stimulation and close with hyperoxia. Any of these happening after a dive could cause DCI when it might not otherwise have occurred; administration of supplemental oxygen is likely to minimize this effect.
Divers With PFO
- The estimated incidence of neurological DCI in divers with PFO is 4.7 DCI cases per 10,000 dives.
- Four studies showed that the prevalence of RLS or a large PFO in divers with spinal DCI is 44% compared to 14.2% in those without either RLS or PFO.
- Half of the divers in the studies with RLS-related DCI have a PFO that is a centimeter in diameter or larger. The highest risk of DCI is in those with the largest PFOs.
- Cerebral, spinal, cutaneous and inner ear DCI are all associated with PFO. The link between PFO and cutaneous and inner ear DCS is the strongest. In approximately 74% of cases with inner ear symptoms and no other symptoms of hyperbaric-related issues, 80% of the cases had a large, spontaneously shunting PFO.
- For a PFO to contribute to DCI, you need to have a large PFO, VGE must form, something must cause the PFO to open, bubbles must cross it, and the bubbles must reach a target tissue while it is still supersaturated and vulnerable.
For more information about PFO, visit Risk Mitigation for Divers With a Known PFO.