Proceedings Summary | DAN/UHMS Diabetes and Recreational Diving Workshop
Introduction
Diabetes is a major chronic disease that affects millions of people worldwide with an increasing trend. In the United States, more than 14 percent of adults are affected. Insulin-dependent diabetes mellitus (IDDM) affects up to half a million people of all ages, out of which 150,000 are younger than 19 years old. Many people continue to be productive members of the community and pursue various interests and careers despite having diabetes. However, when it comes to diving, the diving medicine community has long maintained the conservative position that IDDM is an absolute contraindication for diving. Recognizing that a substantial number of divers are diving successfully (either openly or surreptitiously) with diabetes in spite of the restriction has led many to believe that it is time to acknowledge this fact and re-examine the position concerning diabetes in diving.
A workshop addressing the issues of diabetes and recreational diving was jointly sponsored by the Undersea and Hyperbaric Medical Society (UHMS) and Divers Alert Network (DAN) on June 19, 2005 in Las Vegas, Nevada. They brought together experts and interested parties from within and beyond the international diving community. At the workshop, participants reviewed the existing data, discussed concerns, and finally developed consensus guidelines to address diabetes and recreational diving. The issues concerning professional diving require future, separate deliberations.
The consensus guidelines were released with the clear statement that it is a set of guidelines, not rules and with an understanding that various interest groups must have the flexibility to use the guidelines as they best serve their community’s needs.
This consensus reflects a more inclusive approach and provides guidelines on how to individually evaluate fitness to dive and how to keep it safe for those who qualify. Not everybody with diabetes who wishes to dive will be able to do so; there are various conditions and states of diabetes that would make diving with the condition too risky for divers and for those diving with them.
The guidelines are designed for individual divers who are primarily responsible for their own health and safety. They should adhere to these guidelines developed to improve their protection and that of their dive partners. The guidelines aim to also assist primary physicians and diving physicians evaluating and monitoring divers with diabetes. Other divers should be aware of the guidelines too, and be mindful of special considerations when buddied or leading dives with divers with diabetes.
Who may qualify for recreational scuba diving and how should they be monitored?
Individuals with diabetes who wish to dive must undergo the same medical fitness evaluation as other candidates to ensure first, that no other exclusionary conditions (e.g., epilepsy, pulmonary disease, heart disease, etc.) exist; and second, that there are no complications of diabetes that may increase the risk of injury while diving.
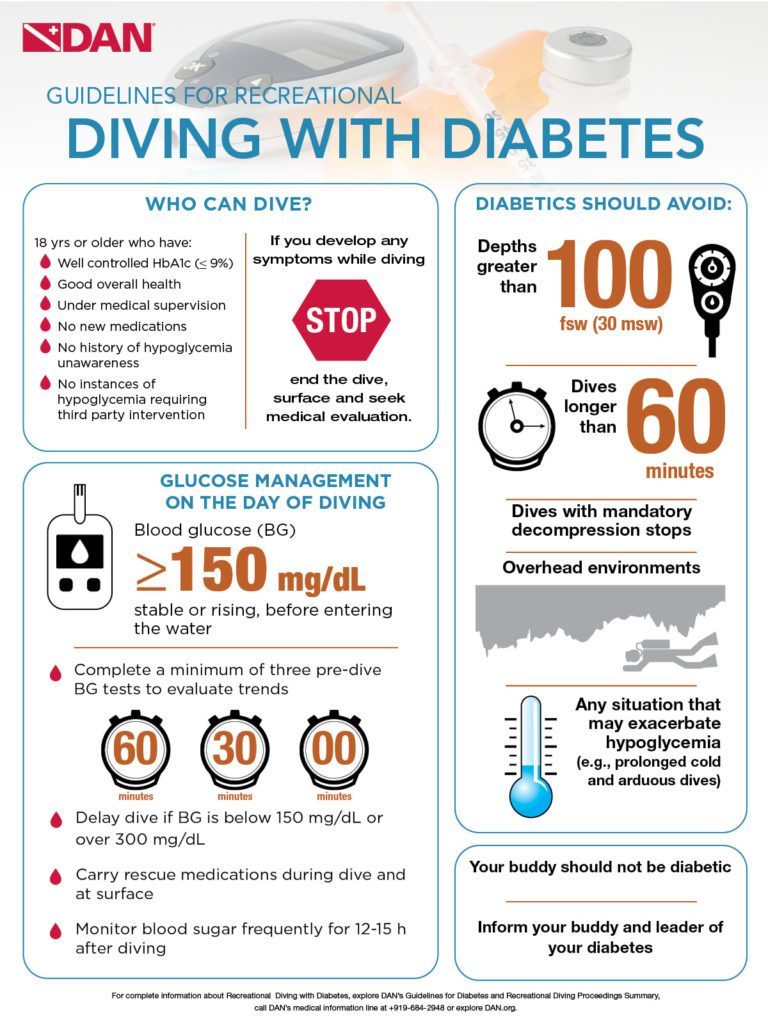
They should be 18 years or older (≥16 years if in special training program), with a well-established treatment, well maintained plasma glucose level and the ability to sustain those levels efficiently in the course of changing demands of daily activities. Candidates and divers with diabetes have to undergo mandatory medical examination annually, and if over 40 years old, they should be regularly evaluated for silent cardiovascular disease.
How to dive with diabetes
Candidates who pass the fitness evaluation and master regular scuba training, must also learn and adhere to the diabetic diving protocol. They should dive only in comfortable environmental conditions, with no overhead. Their dive should not exceed the depth 30 meters of sea water (100 fsw), duration of one hour nor involve compulsory decompression stops.
Divers with diabetes should dive with a buddy who is informed of their condition and is aware of the appropriate response in the event of a hypoglycemic episode. It is recommended that the buddy does not have diabetes.

Glucose management on the day of diving
Divers with diabetes whose medication may put them at risk of hypoglycemia, should use a protocol to manage their health on the day of diving.
- Divers with diabetes should carry oral glucose in a readily accessible and ingestible form at the surface and during all dives. It is strongly recommended that parenteral glucagon is available at the surface. The dive buddy or another person at the surface should be knowledgeable in the use of glucagon. If symptoms or indications of hypoglycemia are noticed underwater, the diver should surface, establish positive buoyancy, ingest glucose and leave the water. An informed buddy should be in a position to assist throughout this process. Use of an “L” signal with the thumb and index finger of either hand is recommended as a signal for suspected hypoglycemia.
- Blood glucose levels should be checked at the end of every dive. Appropriate response to the measured level can be determined by the individual mindful of his or her plans for the rest of the day. It should be noted that the requirements for blood glucose status remain the same for any subsequent dive. In view of the recognized potential for late decrements in blood glucose levels following diving, it is strongly recommended that the level is checked frequently for 12-15 hours after diving.
- Divers with diabetes are strongly recommended to pay particular attention to adequate hydration on days of diving. Elevated blood glucose will lead to increased diuresis. While the data are limited, there is some evidence from divers with diabetes that an increase in hematocrit observed post-dive (suggesting dehydration) can be avoided by deliberate ingestion of fluid.
- Divers with diabetes should log all dives, associated diabetic interventions and results of all blood glucose level tests conducted in association with diving. This log can be used to refine future planning in relation to diving.
Guidelines for recreational diving with diabetes
Selection and Surveillance
- Age ≥18 years (≥16 years if in special training program)
- Delay diving after start/change in medication:
- Three months with oral hypoglycemic agents (OHA)
- One year after initiation of insulin therapy
- No episodes of hypoglycemia or hyperglycemia requiring intervention from a third party for at least one year
- No history of hypoglycemia unawareness
- HbA1c ≤9% no more than one month prior to initial assessment and at each annual review
- values >9% indicate the need for further evaluation and possible modification of therapy
- No significant secondary complications from diabetes
- Physician/Diabetologist should carry out annual review and determine that diver has good understanding of disease and effect of exercise
- in consultation with an expert in diving medicine, as required
- Evaluation for silent ischemia for candidates >40 years of age
- after initial evaluation, periodic surveillance for silent ischemia can be in accordance with accepted local/national guidelines for the evaluation of diabetics
- Candidate documents intent to follow protocol for divers with diabetes and to cease diving and seek medical review for any adverse events during diving possibly related to diabetes
Scope of diving
- Diving should be planned to avoid
- depths >100 fsw (30 msw)
- durations >60 minutes
- compulsory decompression stops
- overhead environments (e.g., cave, wreck penetration)
- situations that may exacerbate hypoglycemia (e.g., prolonged cold and arduous dives)
- Dive buddy/leader informed of diver’s condition and steps to follow in case of problem
- Dive buddy should not have diabetes
Glucose management on the day of diving
- General self-assessment of fitness to dive
- Blood glucose (BG) ≥150 mg·dL-1 (8.3 mmol·L-1), stable or rising, before entering the water
- complete a minimum of three pre-dive BG tests to evaluate trends
- Sixty minutes, 30 minutes and immediately prior to diving
- alterations in dosage of OHA or insulin on evening prior or day of diving may help
- Delay dive if BG
- <150 mg·dL-1 (8.3 mmol·L-1)
- >300 mg·dL-1 (16.7 mmol·L-1)
- Rescue medications
- carry readily accessible oral glucose during all dives
- have parenteral glucagon available at the surface
- If hypoglycemia noticed underwater, the diver should surface (with buddy), establish positive buoyancy, ingest glucose and leave the water
- Check blood sugar frequently for 12-15 hours after diving
- Ensure adequate hydration on days of diving
- Log all dives (include BG test results and all information pertinent to diabetes management)
Pollock NW, Uguccioni DM, Dear GdeL, eds. Diabetes and recreational diving: guidelines for the future. Proceedings of the UHMS/DAN 2005 June 19 Workshop. Durham, NC: Divers Alert Network; 2005.