Jens-Christian Meiners, UMich, Hamilton Award Recipient 2019
Spinal cord decompression sickness is among the most serious forms of decompression illness. It is caused by the growth of gas bubbles in nerve tissue, but how this leads to the observed symptoms is largely unknown. This project studies the mechanics of how bubbles damage the spinal cord by using high-resolution magnetic resonance imaging (MRI) to observe bubble growth and tissue damage in decompressing tissue samples. The goal is to improve recompression treatment.
Spinal cord decompression sickness (DCS) is caused by the growth of inert gas bubbles in the microcapillaries of the spinal cord. It is widely assumed that the pressure associated with these bubbles leads to a local reduction in blood flow and thus the death of the surrounding nerve tissue. Standard recompression treatment of neurological DCS focuses therefore on the reduction of the bubble size and reoxygenation of the tissue. With this project we are exploring a complementary injury mechanism, in which the expanding gas bubble mechanically tears the tissue, resulting in microscopic cuts to nerves in the area. If this hypothesis holds, we need to add another goal to the treatment of spinal cord DCS: promoting the healing of microwounds in the nerve tissue.
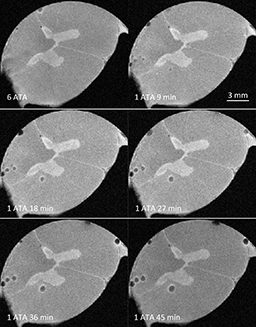
To investigate whether a growing gas bubble can irreversibly tear the surrounding tissue instead of just elastically deforming it, we are studying the mechanical response of spinal cord tissue samples from cows to bubble growth using high-resolution magnetic resonance imaging (MRI). The tissues are saturated with nitrogen at 7 ATA* (198 fsw* / 60 msw*), and then rapidly decompressed to 3 ATA (66 fsw / 20 msw) to induce the formation of decompression bubbles. To ascertain whether further bubble expansion leads to irreversible mechanical damage to the surrounding tissue or just a reversible elastic deformation, we quickly decompress the sample to normal atmospheric pressure and recompress it to 3 ATA. Irreversible tearing will lead to an increased bubble size, as the gas has more space to expand into, whereas a purely elastic reversible deformation would not increase the bubble size upon recompression. Our preliminary data show that after one such decompression/recompression cycle, the bubble volume increases, typically by more than 25%, indicating permanent mechanical tissue damage.
If these findings hold, translation into dive medicine may involve revisiting recompression treatment procedures for neurological DCS to promote healing of microscopic lesions caused by expanding gas bubbles. It may also suggest new avenues for treating non-diving-related traumatic spinal cord injuries using hyperbaric recompression.
*ATA: atmospheres
*fsw: feet of seawater
*msw: meters of seawater
2020 UHMS/DAN Spinal Cord DCS Poster
This study was partially funded through the DAN/R.W. Hamilton Dive Medicine Research Grant in 2019. DAN established the award in honor of Bill Hamilton, Ph.D., a physiologist who conducted important research in decompression science, breathing gases and the effects of pressure. Each year the organization presents the $10,000 grant to a researcher studying decompression stress, models or procedures; mechanisms of decompression illness; dive computer effectiveness; or a similar subject.