Emmanuel Gouin1,2, Emmanuel Dugrenot1,2,3
1: Divers Alert Network (DAN), Durham, NC, USA
2: Univ Brest, ORPHY Laboratory, Brest, France
3: Department of Biomedical Engineering, University of North Carolina at Chapel Hill and NC State, Chapel Hill, NC, USA
Acknowledgments: Dr. Jim Chimiak and Dr. Matias Nochetto (DAN Medical Services, USA) as well as Dr. Sébastien De Maistre (Service de Santé des Armées, France) for their review and comments.
Introduction
During a dive, the cardio-pulmonary changes may provoke an immersion pulmonary edema (IPE/IPO) and increase drowning risk (Castagna et al, 2017). The increase in capillary transmural pressure, influenced by hemodynamic and breathing dynamics, is considered a key factor in the mechanism of IPE (MacIver and Clark, 2015). A combination of stressors and adaptive mechanisms, such as blood shift associated with right to left ventricle imbalance, gas density, hyperoxia, thermal strain, exercise, etc. challenges the respiratory system (Tetzlaff and Thomas, 2017).
Extravascular Lung Water as an IPE Risk Marker
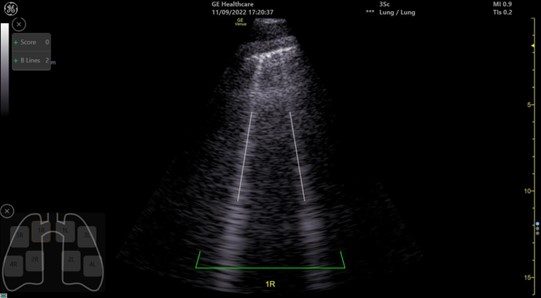
In humans, ultrasonic lung comets (ULC) or B-Lines (Figure 1) have been evidenced after scuba diving and might be related to impaired ventilation related with an accumulation of extravascular lung water (EVLW). Most studies have shown an accumulation of ULC in repetitive deep Open Circuit (OC) dives to 60–80 meters of seawater (msw or 200-260 fsw – feet of sea water), which is not observed at 33 msw (110 fsw) depth (Ljubkovic et al, 2010; Marinovic et al, 2010; Dujic et al, 2011). Conversely, with Closed Circuit Rebreathers (CCR), the lung aeration loss was detected, even in shallow water, between 1 and 10 msw (3.3 and 33 fsw) and was amplified by a moderate fin swimming exercise (Castagna et al, 2017; 2018; Martinez-Villar et al, 2022). The ULC appeared to be transient with a return to the baseline at 24 hours (Gouin et al, 2022).
Rebreathers’ Impact on Pulmonary Function and IPE Risk
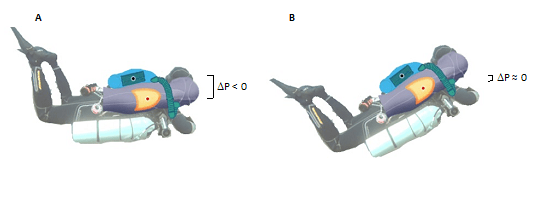
The breathing apparatus by itself may add constraints that influence the static lung load and the work of breathing (WOB). In CCR, the static lung breathing stems from the pressure gradient between the counter lungs and the diver’s lung centroid (i.e., the point of confluence of the forces exerted by the respiratory system). Indeed, in prone position, a back-mounted counter lungs CCR induces a negative pressure breathing (NPB) while the anterior position induces positive pressure breathing (PPB). Castagna has showed that the WOB during immersed activities and the development of interstitial pulmonary edema were more amplified with NPB in comparison to PPB, when the divers are in prone position (Castagna et al, 2018).
To the best of our knowledge, no studies are focusing on the effect of the CCR diver’s position. This position might influence the transpulmonary hydrostatic difference by influencing the pressure gradient (Wilmshurst, 2019), so we hypothesize that a trim position at 30° maximum (as it is usually taught to CCR divers) can reduce the in-water breathing constraints and the negative impact of equipment on the lung during CCR dives. Thus, this trim position might reduce the risk of IPE occurrence and could be encouraged in CCR community while open-circuit divers promote the prone position (Figure 2). Therefore, more studies are needed on this topic.
As previously mentioned, Gouin et al, (2022) study on CCR divers evaluated the cardiopulmonary impact of repeated back mounted CCR dives. During that study, they followed 8 CCR divers on a one-week diving trip in the Baltic Sea, and measured, among other things, spirometry parameters, oxygen saturation (SpO2), Heart Rate Variability (HRV), and lung ultrasonography score (LUS), which reflects possible extravascular lung water.
Interestingly, if they did observe transient increased LUS after diving combined with a slight non-pathological decrease in oxygen saturation (SpO2), it did not seem to correlate with depth, while the dives were up to 230 fsw or 70 msw (Figure 3).
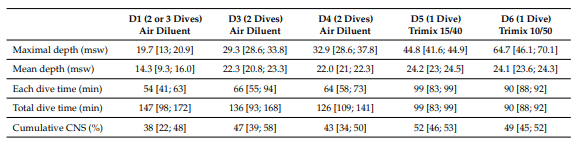

In that study, the lung aeration disorders observed seem to be transient and not associated with functional alteration. This implies the impact of these impairments is unknown and should not be neglected until we better understand IPE physiopathology and the decrease in Forced Vital Capacity (FVC, which is a pulmonary function marker) observed during deeper CCR dives (Dugrenot et al, 2021). Further studies are needed on these two topics.
Besides these cardiopulmonary parameters, Gouin et al (2022) also collaborated in another study focused on the inflammatory pathway related to decompression sickness (DCS), more precisely on circulating microparticles, which are known to initiate a systemic inflammatory response. These microparticles were indeed increased after a deep CCR dive or after repetitive shallow CCR dives, highlighting that inflammatory events are decorrelated from the depth of diving, and might also impact lung function (Arya et al, 2023).
IPE Risk Factors
Well supported risk factors of IPE are: being over 50 years old, being a female, non-steroidal anti-inflammatory drug (NSAID) intake before diving, physical exertion prior to or during the dive, increased work of breathing (which will be affected by gas density), tight suit/equipment, cold water and arterial hypertension (Henckes et al, 2019; Wilmshurst, 2019). Some other factors, like overhydration, have also been cited (Edmonds et al, 2019). However, none of the statistics from the studies cited above have been able to confirm this.
Before drawing any conclusions, it is important to remember that even exercise itself can cause the appearance of B-lines, even on healthy subjects (Simonovic et al, 2018). Pressure variations could also impact B-line formation (Debevec et al, 2022). Moreover, negative pressure itself can trigger IPE (Bhattacharya et al, 2016) and even laryngospasm can draw fluids from pulmonary capillaries and trigger pulmonary edema (Andersen et al, 1988). Similarly, an increased inspiratory resistance caused by a poorly calibrated regulator may cause a transient sub-ambient pressure (negative pressure breathing) that could play a role in it the pathogenesis of IPE. This highlights the importance of a well set ADV (Automatic or Added Diluent Valve) and proper Optimal Loop Volume management, and even raises the question of a mandatory use of the ADV for training and exploration.
Glossary
CCR: Closed Circuit Rebreathers
EVLW: extravascular lung water
Fsw: feet of salt water
FVC: Forced Vital Capacity
HRV: Heart Rate Variability
IPE/IPO: Immersed Pulmonary O(E)dema
LUS: lung ultrasonography score
Msw: meters of sea water
NPB: negative pressure breathing
NSAID: non-steroidal anti-inflammatory drug
OC: Open Circuit
PPB: positive pressure breathing
SpO2: oxygen saturation
ULC: ultrasonic lung comets
WOB: work of breathing
References
Andersen, C., C. B. Kancir, and K. D. Nielsen. “Laryngospasm‐induced Pulmonary Oedema.” Acta Anaesthesiologica Scandinavica 32, no. 8 (November 1988): 710–11. https://doi.org/10.1111/j.1399-6576.1988.tb02813.x.
Arya, Awadhesh K., Costantino Balestra, Veena M. Bhopale, Laura J. Tuominen, Anne Räisänen-Sokolowski, Emmanuel Dugrenot, Erwan L’Her, Abid R. Bhat, and Stephen R. Thom. “Elevations of Extracellular Vesicles and Inflammatory Biomarkers in Closed Circuit SCUBA Divers.” International Journal of Molecular Sciences 24, no. 6 (March 22, 2023): 5969. https://doi.org/10.3390/ijms24065969.
Bhattacharya, Mallar, Richard H. Kallet, Lorraine B. Ware, and Michael A. Matthay. “Negative-Pressure Pulmonary Edema.” Chest 150, no. 4 (October 2016): 927–33. https://doi.org/10.1016/j.chest.2016.03.043.
Castagna, Olivier, Emmanuel Gempp, Raphael Poyet, Bruno Schmid, Anne-Virginie Desruelle, Valentin Crunel, Adrien Maurin, Romain Choppard, and David H. MacIver. 2017. ‘Cardiovascular Mechanisms of Extravascular Lung Water Accumulation in Divers’. The American Journal of Cardiology 119 (6): 929–32. https://doi.org/10.1016/j.amjcard.2016.11.050.
Castagna, Olivier, Jacques Regnard, Emmanuel Gempp, Pierre Louge, François Xavier Brocq, Bruno Schmid, Anne-Virginie Desruelle, et al. 2018. ‘The Key Roles of Negative Pressure Breathing and Exercise in the Development of Interstitial Pulmonary Edema in Professional Male SCUBA Divers’. Sports Medicine – Open 4 (1): 1. https://doi.org/10.1186/s40798-017-0116-x.
Dugrenot, Emmanuel, Costantino Balestra, Emmanuel Gouin, Erwan L’Her, and François Guerrero. “Physiological Effects of Mixed-Gas Deep Sea Dives Using a Closed-Circuit Rebreather: A Field Pilot Study.” European Journal of Applied Physiology 121, no. 12 (December 2021): 3323–31. https://doi.org/10.1007/s00421-021-04798-y.
Edmonds, Carl, John Lippmann, and Alfred Bove. “Immersion Pulmonary Edema: An Analysis of 31 Cases from Oceania.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc 46, no. 5 (December 2019): 603–10.
Debevec, Tadej, Mathias Poussel, Damjan Osredkar, Sarah J. Willis, Claudio Sartori, and Grégoire P. Millet. “Post-Exercise Accumulation of Interstitial Lung Water Is Greater in Hypobaric than Normobaric Hypoxia in Adults Born Prematurely.” Respiratory Physiology & Neurobiology 297 (March 2022): 103828. https://doi.org/10.1016/j.resp.2021.103828.
Dujic, Zeljko, Jasna Marinovic, Ante Obad, Vladimir Ivancev, Toni Breskovic, Pavle Jovovic, and Marko Ljubkovic. 2011. ‘A No-Decompression Air Dive and Ultrasound Lung Comets’. Aviation, Space, and Environmental Medicine 82 (1): 40–43. https://doi.org/10.3357/ASEM.2868.2011.
Gouin, Emmanuel, Costantino Balestra, Jeremy Orsat, Emmanuel Dugrenot, and Erwan L’Her. 2022. ‘Pulmonary Effects of One Week of Repeated Recreational Closed-Circuit Rebreather Dives in Cold Water’. Medicina 59 (1): 81. https://doi.org/10.3390/medicina59010081.
Henckes, Anne, Guy Cochard, Florence Gatineau, Pierre Louge, Emmanuel Gempp, Sébastien Demaistre, Emmanuel Nowak, and Yves Ozier. “Risk Factors for Immersion Pulmonary Edema in Recreational Scuba Divers: A Case-Control Study.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc 46, no. 5 (December 2019): 611–18.
Ljubkovic, Marko, Svein Erik Gaustad, Jasna Marinovic, Ante Obad, Vladimir Ivancev, Nada Bilopavlovic, Toni Breskovic, Ulrik Wisloff, Alf Brubakk, and Zeljko Dujic. 2010. ‘Ultrasonic Evidence of Acute Interstitial Lung Edema after SCUBA Diving Is Resolved within 2–3h’. Respiratory Physiology & Neurobiology 171 (2): 165–70. https://doi.org/10.1016/j.resp.2010.02.008.
MacIver, David H., and Andrew L. Clark. 2015. ‘The Vital Role of the Right Ventricle in the Pathogenesis of Acute Pulmonary Edema’. The American Journal of Cardiology 115 (7): 992–1000. https://doi.org/10.1016/j.amjcard.2015.01.026.
Marinovic, Jasna, Marko Ljubkovic, Ante Obad, Toni Breskovic, Ilza Salamunic, Petar J. Denoble, and Zeljko Dujic. 2010. ‘Assessment of Extravascular Lung Water and Cardiac Function in Trimix SCUBA Diving’. Medicine & Science in Sports & Exercise 42 (6): 1054–61. https://doi.org/10.1249/MSS.0b013e3181c5b8a8.
Martinez-Villar, María, Antonio Tello-Montoliu, Agustín Olea, Ángel Pujante, Daniel Saura, Silvia Martín, Nereo Venero, et al. 2022. ‘Global Longitudinal Strain Assessment of Cardiac Function and Extravascular Lung Water Formation after Diving Using Semi-Closed Circuit Rebreather’. European Journal of Applied Physiology 122 (4): 945–54. https://doi.org/10.1007/s00421-022-04887-6.
Simonovic, Dejan, Stefano Coiro, Erberto Carluccio, Nicolas Girerd, Marina Deljanin-Ilic, Gaia Cattadori, and Giuseppe Ambrosio. “Exercise Elicits Dynamic Changes in Extravascular Lung Water and Haemodynamic Congestion in Heart Failure Patients with Preserved Ejection Fraction: Exercise Elicits Dynamic Changes in Extravascular Lung Water and Haemodynamic Congestion in Heart Failure Patients with Preserved Ejection Fraction.” European Journal of Heart Failure 20, no. 9 (September 2018): 1366–69. https://doi.org/10.1002/ejhf.1228.
Tetzlaff, Kay, and Paul S. Thomas. 2017. ‘Short- and Long-Term Effects of Diving on Pulmonary Function’. European Respiratory Review 26 (143): 160097. https://doi.org/10.1183/16000617.0097-2016.
Wilmshurst, Peter T. “Immersion Pulmonary Oedema: A Cardiological Perspective.” Diving and Hyperbaric Medicine Journal 49, no. 1 (March 31, 2019): 30–40. https://doi.org/10.28920/dhm49.1.30-40.