Q: On a recent dive trip, my buddies and I dived using 30 percent nitrox. Beyond our maximum operating depth was a big turtle that my buddies wanted to photograph. They decided to take deep breaths and hold them to prevent breathing in oxygen at the deeper depth. Besides the obvious concerns regarding breath-holding and exceeding maximum operating depth, I thought the oxygen in a diver’s system would be compressed to ambient pressure regardless of whether or not he breathed. Can you please clarify?
As you surmise, the logic employed by the other divers was not valid. The gas in their lungs would be compressed as they descend, whether or not they breath-hold. Descent produces an increase in the gradient that drives oxygen into the blood, and the volume of gas in the lungs is substantial enough that constant breathing is not required for the effect to be meaningful.
The risk of oxygen toxicity also increases with increasing exercise intensity and carbon dioxide (CO2) levels. Thus, not only did these divers fail to eliminate the elevated oxygen exposure, but also the breath-hold would have created rising CO2 levels to further increase the risk of toxicity if sustained for a substantial period of time.
The question of what is an appropriate maximum partial pressure of oxygen (PO2) has evolved recently. The old limit of 1.6 ATA has largely been replaced with 1.4 ATA, particularly for depths where the complication of a seizure would be much more difficult to survive. One of the most challenging realities to understand in diving physiology is that getting away with something once, twice or 10 times is not a guarantee of future safety. Respecting maximum operating depths to limit PO2 to no more than 1.4 ATA and keeping exercise intensity at depth as low as possible should be the baseline for safe practice. Creative alternatives may be enticing right up to the point where they fail. The best way to prioritize safety is to adopt more conservative limits wherever feasible, and bear in mind, in real time, that the worst possible outcomes really can happen. Our diving fatality databases make this unhappy truth very clear.
— Neal Pollock, Ph.D.
Q: My doctor recently diagnosed me with mild COPD. Can I still dive with this condition? What are the risks?
Chronic obstructive pulmonary disease (COPD), also known as chronic obstructive lung disease (COLD), encompasses a variety of respiratory health problems, including chronic bronchitis and emphysema. Regardless of what form of COPD a person may have, there are implications for diving and risks of which the person should be aware.

Chronic bronchitis is defined clinically as a productive cough that persists for periods of up to three months and occurs one or more times a year for at least two years. During these periods, the risk of infection, including pneumonia, is high. The inflammation of the bronchial passages and increased mucus production that characterize these periods are uncomfortable: Patients report wheezing, difficulty breathing and feeling as though they cannot get enough air.
For divers, the inflammation and excess mucus lead to the possibility of trapping dense compressed gas at depth. Upon ascent the gas will expand in volume, potentially leading to pulmonary barotrauma, which could include pneumothorax (collapsed lung) and, in the worst case, arterial gas embolism (AGE). Of these, AGE is the most immediate threat to life, but a complicated pneumothorax can also be fatal.
Emphysema is defined clinically as permanent abnormal enlargement of the air spaces within the lungs due to the deterioration of the alveoli. These enlarged spaces are conducive to trapping air at depth, which creates the same possibility of pulmonary barotrauma as chronic bronchitis.
For medical management purposes with regard to medications and other therapies, physicians classify COPD as mild, moderate, severe or very severe, as determined by severity of airflow obstruction. Even with the clinical designation of mild there is measurable obstruction beyond what is considered safe among pulmonology experts trained in dive medicine. For these reasons, diving with COPD — even mild COPD — is not recommended.
— Marty McCafferty, EMT-P, DMT
Q: I have heard that it’s not uncommon for hyperbaric chambers — even ones that treat divers — to refuse to receive certain patients. Why is this?
We are aware of this issue, which we recently discussed in an open forum at the Undersea and Hyperbaric Medical Society Gulf Coast Chapter meeting. We have also written articles about the growing number of chambers that do not accept emergency cases. The following are some of the reasons why hyperbaric chambers might refuse patient transfers:
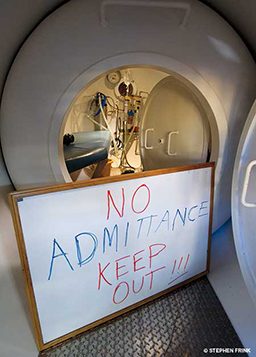
- Availability: Sometimes there simply are not enough chambers. For example, a facility may already have a patient in a chamber and not have the staff or chamber space to manage others. If a small facility accepts an emergency case, that could force the facility to reschedule or cancel scheduled treatments due to the longer periods of time required for emergency care. Even if a chamber can admit a patient, the hospital or clinic might not have any beds available, which precludes acceptance of some patients.
- Staffing: Many facilities lack 24-hour on-call coverage. Smaller facilities may have only one or two physicians, who may be mainly employed in other specialties, such as primary care or emergency medicine. Tender and technician positions may also be limited in smaller facilities. The comfort level of the physicians with a particular case must also be considered. A physician who has treated only stable divers, for example, may not feel comfortable enough with his or her expertise to provide care in a serious case of decompression illness.
- Patient condition: Certain facilities are not equipped to accept critically injured patients. For example, a patient on a ventilator could not be adequately treated in a facility designed for stable patients. Even though large multiplace facilities are more likely to be able to accept emergency cases, the facility would have to be equipped with critical-care capabilities.
There are so many pieces to this puzzle that one cannot always assume that a facility is willfully refusing to treat patients. In the event of an emergency, call DAN; we’re committed to helping you get the care you need.
— Scott Smith, EMT-P, DMT
Q: My next dive trip is taking me across the world. Whenever I cross time zones, I suffer relatively severe jet lag, which affects my ability to dive safely. What might I do to minimize the effects of jet lag?
Long-distance air travel that crosses several time zones causes jet lag syndrome because our circadian rhythms are out of sync with the time at the destination. Symptoms include fatigue, hunger and alertness at the wrong times of day. Fortunately, within a few days our internal clock tends to synchronize with the environment. The more time zones we cross, the greater the expression of the syndrome and the longer it takes to overcome.
To minimize the effects of jet lag, try the following strategies:
- Prepare: Before your trip, try to move your bedtime gradually to what it will be at your intended destination. For eastward travel, take one day to go to bed one hour earlier than normal for each time zone you will cross. To make it easier to fall asleep early, avoid caffeine and alcohol, and don’t exercise within three or four hours of bedtime. Get up earlier, and try to catch some morning sunshine to help your body adjust. When preparing to travel west, go to bed later and stay in bed longer.
- Sleep in flight: Losing sleep during your flight exaggerates the effects of rapid time zone change. During sleep, your body temperature falls, and the activity of some of your hormones changes. With the onset of darkness at night, the pineal gland in the brain starts secreting the hormone melatonin, which helps the body fall and stay asleep. Melatonin, however, is not strong enough to put you asleep on its own. To sleep during the flight, avoid alcohol and caffeine, which keep you alert, and use earplugs and blindfolds to reduce noise and mimic nighttime darkness. If that is not enough, you can use 0.3 to 1 mg of melatonin 30 minutes before bedtime.
- Adhere to a schedule: Upon arrival at your destination, try to stay active during daylight hours and go to bed in the evening at your usual time. In the morning, go out into the sunlight to help adjust your circadian rhythm. Of course, if you travel from a geographic area where it is summer to a geographic area where it is winter, this may not be possible; instead, try to start your morning in a gym or swimming pool.
Melatonin is available as an over-the-counter product classified as a food supplement, which means it is not regulated. The amount of active hormone in one pill may vary slightly from what is declared on the box, and some people may need more or less melatonin to feel its effects. Be aware that too much melatonin can actually have the opposite of the intended effect and interfere with your sleep. A good rule of thumb when it comes to melatonin is to avoid taking more than 3 mg at once. While it is considered nonaddictive and safe for short-term use, too much melatonin can also cause headaches, nausea, dizziness or irritability, and it can interact with various medications, including anticoagulants, immunosuppressants, diabetes medications and birth-control pills. If you have any health conditions, check with your doctor before using melatonin.
Diving on the first day at your destination is probably not a good idea after a long trip. To be well rested for the next day’s diving, you may take melatonin at bedtime. It is not advised to engage in activities that require alertness, such as diving or driving, for four to five hours after taking melatonin. This means that if you arrive at your destination late at night and take melatonin after midnight, you should probably abstain from the first morning dive.
— Petar Denoble, M.D., D.Sc.
© Alert Diver — Q1 Winter 2015