Patent foramen ovale (PFO) is a passage through the wall that separates the left and right fore chambers (atria) of the heart. During the intrauterine period of life, the PFO enables proper circulation while the lungs are closed. After birth, this path is sealed in most people, but in about 25 percent of the population it may still occasionally open if the pressure in the right atrium exceeds the pressure in the left atrium. In about 1 percent of people there may be an incomplete closure, which leaves a permanent hole in the atrial wall and enables blood to flow through on a regular basis.
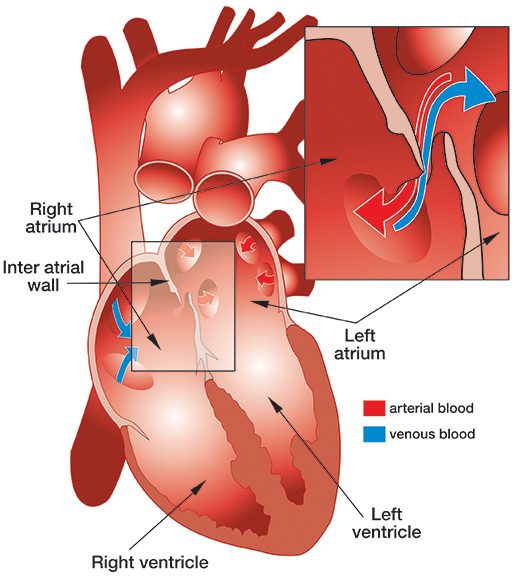
PFO is a suspected risk factor for decompression sickness (DCS), but a causative relationship between PFO and DCS has not been clearly established. It seems plausible that bubbles may bypass the lungs, which usually filter them out, by traveling directly from the right atrium to the left atrium through the PFO. For this to happen, two conditions must be present: The dive must result in circulating venous bubbles and the PFO must be open. A PFO opens on rare occasions such as when divers lift heavy weights, squat or employ the Valsalva maneuver (an equalization technique).
Bubbles are probably present after most dives but are more likely after longer or deeper dives. That being said, some divers experience DCS after apparently innocuous dives, including some who have tested positive for PFO. The more bubbles there are and the more blood that passes through the PFO, the more likely the diver would be to develop DCS.
Most statistics indicate the risk of DCS in divers with PFO may be several times greater than in divers without PFO, but the risk is still very small. Thus, there is no need to test every scuba diving candidate for a PFO. However, some doctors may want to administer the PFO test if a diver has a history of DCS; currently there is no established consensus on what actions should be taken if the diver tests positive.
In light of the suspected increased risk of DCS, if divers test positive for PFO, they may choose to stop diving or take steps to mitigate their risks in the future. While the risk assessment and acceptability varies from case to case, divers may be advised either to dive more conservatively to minimize chances for an occurrence of venous bubbles or to close the PFO to prevent passage of the bubbles to the arterial side. The risk-benefit of continuing diving with or without closure has not been established.
To address this question DAN has established a PFO study, which started in 2010 and will continue for five years. The study will enroll 120 qualified participants with annual follow ups throughout its course. As of this writing, there are 30 subjects enrolled in the study. We’ve explored their dive histories and reasons for testing and conducted a comparison of divers who underwent closure to those who did not. This is what we’ve found thus far.
Dive history
Of the 30 enrolled participants, 21 divers who frequently practiced deep and decompression diving and one professional diver reported dive practices that likely resulted in the generation of a substantial amount of venous gas bubbles. The other eight divers reported diving within typical recreational no-decompression limits.
History of DCS
Nineteen divers suffered repeat episodes of DCS, while eight had a single episode. In the remaining three divers, the PFO was found during another cardiac procedure. Of these three, one had a 7 millimeter hole, an atrial septal defect (ASD); she had conducted 150 dives prior to her surgery with no incidence of DCS. The other two divers each had over 800 dives and no incidence of DCS.
Some divers reported feeling that their DCS was “undeserved,” but most dive histories contained dives with a significant potential to produce venous gas bubbles.
DCS Manifestations
- Sixteen divers reported at least one instance of DCS with symptoms reflecting affliction of more than one organ. The typical bundle of symptoms included skin changes, fatigue, chokes, confusion or vertigo in any combination.
- Six divers had a history of single organ symptoms including two cases each of vestibular, skin and leg weakness.
- Five divers reported only ambiguous symptoms; two of these divers requested tests to conform to requirements of particular dive groups.
- One diver was diagnosed with a large PFO and underwent closure; although in his five years of diving and 280 dives, he never experienced any post-dive symptoms.
- The remaining two divers had a history of false alarms regarding DCS symptoms and requested testing to address their concerns.
The Size of the Shunt
Since the methods of quantifying the volume of shunted blood in PFO vary, they could not be compared. Six of the participating divers had either ASD and/or an atrial septal aneurysm (ASA).
Closure vs. Non-Closure
Nineteen out of 30 study participants underwent PFO closure; 14 out of 24 divers with a simple PFO and five out of six divers with ASD or ASA. When comparing the dive practices between the closure and non-closure groups, they did not differ significantly suggesting that it may not have been a deciding factor for most of the divers who underwent closure. However, the DCS history of the closure group revealed more divers who had experienced at least one episode of DCS affecting multiple organs or a repetitive occurrence of DCS (18 out of 19 divers compared to 4 out of 11 divers in the non-closure group).
Summary
The dive and DCS history in most of our participants justified for PFO testing, but few seem to have requested testing for different reasons. A positive PFO test is a marker of an increased risk of DCS and having confirmed diagnosis may help divers to focus on proper mitigation measures. By the end of the study, we hope to learn about the risk-benefit of various mitigation measures. Divers who suffer DCS with symptoms affecting multiple organs, severe neurological DCS or repeated skin bends should consider testing for PFO.
© Alert Diver — Q2 Spring 2010