“Dive conservatively” has become advice recreational divers commonly receive. It is frequently followed by generic instructions such as don’t push the no-decompression limits, use nitrox, limit your depth, do not exert yourself underwater, be hydrated or stay warm. The apparent intent of this advice is to reduce the risk of decompression sickness (DCS). To dive conservatively seems like common-sense advice with regard to decompression safety, but the efficacies of the suggested strategies are generally not known, and methods for their evaluation are not available.
To better understand how divers can be more conservative in their choices, let’s consider how the current decompression rules were constructed and how effective they are.
Beyond Trial and Error
The history of diving is a history of trials and errors. A modern scientific approach was introduced in the development of decompression procedures at the turn of 20th century. The trial-and-error methods became less futile, and the human toll of their failures was reduced to acceptable levels thanks to the use of efficacy studies and effectiveness studies.
Efficacy studies aim to establish whether a particular decompression procedure works and to determine the limits of its safe use. This can be done only in prospective studies in strictly controlled experimental environments. The gold standard of efficacy studies in diving research is human decompression trials. Such trials were conducted at the U.S. Navy Experimental Diving Unit (NEDU) and the Canadian Defense and Civil Institute of Environmental Medicine (DCIEM) and evaluated several generations of U.S. Navy and Canadian decompression tables. Similar studies were conducted by the French Navy and Royal British Navy as well as some other navies and, to some extent, by Dr. Albert A. Bühlmann, M.D., in Zurich, Switzerland.

Effectiveness studies, on the other hand, evaluate real-life implementations of experimentally verified decompression methods. They are based on real-world data. One example of an effectiveness study, although it was not called that at the time, is a retrospective evaluation of 16,170 dives recorded at the U.S. Naval Safety Center for the years 1971 to 1978.1 These real-world data were not available for all decompression schedules covered by the decompression tables. Only 43 of the 295 U.S. Navy air decompression schedules were used 100 times or more during the seven-year period, and half of the schedules were not used at all. The overall incidence rate of DCS was 1.25 percent; the incidence rate for schedules with more than 50 dives ranged from 0 percent to 4.8 percent. In general, the longer the dive, the higher the incidence of DCS. Although the tables were developed based on empirical data, the number of depth-time profiles tested and the number of trials were limited; thus, the generalized model resulted in less-than-desirable safety in some schedules.
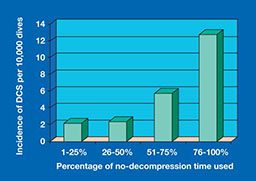
Another example of an effectiveness study is a 1998 evaluation by the U.S. Naval Medical Research Institute of real-world data pertaining to no-stop decompression dives reported to the U.S. Naval Safety Center.2 The data consisted of 163,400 shallow dives (made in 21 to 55 feet of seawater and within no-decompression limits) and 48 cases of DCS reported from 1990 to 1994. The overall incidence rate for DCS was 2.9 per 10,000 dives (0.029 percent). When the dive time was 25 percent of the allowed no-decompression time, DCS occurred in only one out of 10,000 dives (0.01 percent), and it increased to four out of 10,000 dives (0.04 percent) when more than 75 percent of the allowed time was used.
Applying Decompression Models to Recreational Diving
Since those studies, the U.S. Navy has conducted several series of human trials and has developed more efficient models, but these were all designed primarily for Navy use. The Navy trials measured outcomes of DCS symptoms, and the targeted probability of DCS was 2 percent or less with 90 percent confidence that probability was less than 5 percent. This approach is impractical for evaluating models designed for recreational diving, which should keep DCS risk at less than 1 percent (i.e., a probability of DCS less than 0.01). To test models with such a low probability of DCS, even 100 symptom-free dives per schedule would not be enough. To prove with 90 percent confidence that probability is less than 0.01, the trial should include nearly 300 dives. And this is for just one point on the matrix of schedules that would have to be covered to thoroughly test a decompression model.
In its human trials the Canadian DCIEM used a surrogate outcome: venous gas emboli (VGE), which occur more often than DCS symptoms and enable testing of models with a lower risk of DCS. While the link between VGE grade and DCS onset is not straightforward, a grade of VGE 2 or below is associated with a very safe dive. DCIEM tables were designed to keep VGE (and, thus, DCS risk) low. This method may be more appropriate for models developed for recreational diving. However, it is still complex to compute and prohibitively expensive for most manufacturers in the recreational dive market.
Decompression models like those of the U.S. Navy and DCIEM, whose efficacy was tested in human trials, are known as primary models. With the exception of the Bühlmann tables, most decompression tools used in contemporary recreational diving — whether they are modified military tables or newly developed models — were not subject to systematic human trials and do not have efficacy data. They are secondary models, which refer to primary models for their safety margins. With regard to allowable bottom times and prescribed decompression times, these models vary between “liberal” U.S. Navy and “conservative” DCIEM prescriptions. Such calibration can easily be done for simple square dives, but when it comes to multilevel, repetitive and multiday diving in a variety of environmental conditions, this method is far from reliable.
In general, users of dive computers have the option to set their computers to be less or more conservative. This is based on theoretical assumptions that the risk of DCS can be predictably diminished by limiting bottom time, slowing ascent, adding decompression stops and increasing the partial pressure of oxygen. While these techniques work most of the time, voluntary variation of computing parameters may bend and tweak the decompression curve in unpredictable ways and lead to unwanted outcomes. Fortunately, most recreational dives occur within parameters of low enough DCS risk that erroneous models will not usually cause harm to divers. When it comes to more serious diving, untested assumptions and erroneous computation may result in serious injuries.

Risk Management for Tomorrow’s Divers
The public is becoming more aware that guesses and assumptions cannot replace evidence-based approaches when safety is at issue. Unfortunately, the likelihood is diminishing that human trials will be used for evaluating recreational diving practices. Modern society prohibits trials with humans or animals unless the problem to be solved exceeds the potential harm to the study subjects. Given the low overall risk of DCS, testing the new decompression models to their limits would expose trial subjects to higher-than-usual risks with the prospect of only a small gain for society. On the other hand, if advances in decompression safety depend only on existing experimental data, new computing technologies that become available won’t be implemented to their full potential.

Unlike experimental studies, real-world data are widely available and can be used to evaluate how effectively certain decompression methods prevent DCS in real life. Real-world data may be used to evaluate the effectiveness of a single procedure with known efficacy or, as is most often case, for comparative-effectiveness research to compare two different methods for treating the same condition.
An example of retrospective comparative-effectiveness research is a recently published study about the incidence of DCS after the recommendation of conservative decompression practices to divers with and without vascular right-to-left shunts.3 The study group included 27 divers who were advised to dive conservatively due to the presence of a right-to-left shunt — including patent foramen ovale (PFO) — or due to a previous history of DCS. “Diving conservatively” in this context meant reducing the nitrogen load by limiting dive depth and/or dive time and/or using nitrox.
Before the intervention, the 27 divers performed 17,851 dives and reported 34 cases of DCS — an incidence of 19 cases per 10,000 dives, which is much higher than the average of 2 to 4 cases per 10,000 dives seen in the recreational diving population. After they were given recommendations to dive conservatively, researchers followed the divers for an average of 5.3 years. In that period the subjects performed 9,236 dives and reported four cases of DCS (4.3 per 10,000 dives — a nearly fourfold decrease compared to the pre-intervention period). This study indicates that recommendations to reduce nitrogen load work for divers who were apparently at increased risk for DCS due to the presence of a PFO or other unknown factors. The risk of suffering recurrent DCS after a recommendation to dive conservatively became similar to the average risk in the recreational diving population.
In the future we may see more comparative-effectiveness research comparing various dive computers and diving practices to one another or to a selected standard. Divers should have enough information to choose their dive profiles with confidence. So far, the first comparative-effectiveness study of conservative diving seems to justify the concept, but more quantitative studies are needed.
References
- Berghage TE, Durman D. U.S. Navy Air Decompression Schedule Risk Analysis. Naval Medical Research Institute, Report 80-1. Bethesda, Md., 1980.
- Flynn ET, Parker EC, Ball R. Risk of decompression sickness in shallow non-stop air diving: an analysis of Naval Safety Center data for 1990–1994. NMRI 1998-08. Bethesda, Md., 1998.
- Klingmann C, Rathmann N, Hausmann D, Bruckner T, Kern R. Lower risk of decompression sickness after recommendation of conservative decompression practices in divers with and without vascular right-to-left shunt. Diving Hyperb Med. 2012 Sept; 42(3):146-50.
© Alert Diver — Q3 Summer 2013