The breathing of compressed gas while submerged and exposed to increased ambient pressure imposes significant homeostatic challenges on the body (i.e., challenges maintaining physiological equilibrium). This article discusses the important mechanisms of these challenges, with particular attention to the respiratory system.
I. THE RESPIRATORY SYSTEM
Compressed-Gas Breathing Equipment

Scuba equipment is the most commonly used recreational compressed-gas system, and it provides examples of important features and functions relevant to diving physiology. Basic scuba equipment consists of a cylinder of air at high pressure, a demand-valve regulator and a device for holding this equipment on the diver’s back, typically a buoyancy control device (BCD). Together with a wetsuit (necessary for temperate-water diving) and a weight belt, this apparatus may constitute a significantly restrictive force over the diver’s chest and abdomen.
The regulator reduces the high-pressure air in the cylinder to ambient pressure and supplies air on demand. Thus, at a depth of 100 feet, where the absolute pressure is 4 atmospheres, the regulator supplies air at 4 atmospheres, and the air is four times as dense as air at sea level (1 atmosphere). The ambient pressure is measured by the regulator’s second stage (attached to the mouthpiece), which in an upright diver is approximately 8 inches above the center of the chest. The water pressure acting on the chest will therefore be approximately 8 inches of water depth greater than that of the inspired gas, creating negative transmural pressure (pressure difference across the chest wall) that’s greatest at the base of the lungs.
The breathing resistance of a regulator is inversely related to the quality of manufacture and standard of maintenance. Furthermore, breathing resistance tends to increase with depth as denser air flows through the regulator mechanism.
Finally, it should be noted that the internal volume of a portion of the regulator second stage is effectively an extension of anatomical respiratory dead space.
Mechanics of Diving
Changes in compliance: Changes in compliance are seen in the lungs and chest wall. The negative transmural pressure across the chest wall of the upright scuba diver causes some pulmonary capillary engorgement. This effect is enhanced by the relative centralization of blood volume that occurs with immersion, especially in cold water. This engorgement of the pulmonary capillaries causes reduced compliance in the lung tissue. This reduces the vital capacity of the lung by 10-15 percent.
Scuba equipment, wetsuits and weight belts exert a restrictive force on the chest wall and abdomen. This effect is potentially significant if equipment is excessively tight fitting. The compliance of the chest wall is reduced, and diaphragmatic breathing is impeded.
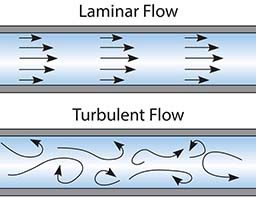
Changes in airways resistance: Airways resistance is affected by changes in gas density. Resistance is defined as the pressure decrease across a tube divided by flow. In laminar flow, flow is largely independent of the density of the gas. In turbulent flow, however, flow is inversely related to gas density. Therefore, in turbulent flow, for a given pressure decrease, flow will be decreased if gas density is increased, and by definition resistance to flow will be greater.
According to Reynolds number predictions (a method of predicting flow), flow within the lungs and airways is largely laminar; this assumption, however, is likely to be invalid because of the vortices that occur in inspired air at each division of the bronchial tree. Indeed, it is likely that turbulent flow occurs widely in the large airways, particularly during rapid breathing when flow rates are much higher.
Changes in the work of breathing: Work of breathing in diving is consequently increased. Work is performed by the respiratory muscles in stretching the elastic tissues of the lungs and chest wall, moving inelastic tissues and moving air through the respiratory passages. The preceding discussion demonstrates that in the immersed scuba diver there is an increase in elastic work (due to decreased compliance in the lungs and chest wall), work of moving inelastic tissues (due to constrictive equipment) and work of moving air through airways (due to increased air density). The airways-resistance component of this increase in work of breathing is dependent upon depth.
Ventilation/Perfusion Matching the Diving
The single most important determinant of efficient gas exchange is the matching of alveolar ventilation to the perfusion of the alveolar capillaries. The optimum ratio of these two factors is unity. Underveentilated and overperfused lung units represents a right-to-left shunt.
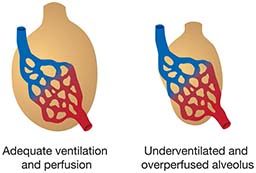
The mixture of hypoxic blood from underventilated and/or overperfused units into systemic arterial blood is an important cause of a significant alveolar-arterial oxygen gradient.
The lungs of a scuba diver are subjected to changes in both perfusion and ventilation. There is an increase in perfusion of lung units due to capillary engorgement (particularly at the bases of the lungs) and the relative centralization of blood volume that occurs with immersion. There is a decrease in ventilation due to reduced lung- and chest-wall compliance, abdominal constriction and increased airways resistance. The net effect is toward an increase in underventilated and/or overperfused units and thus the shunting of blood from right to left.
Changes in Gas Transport
Oxygen: Oxygen is transported in the blood either bound to hemoglobin (Hb) or dissolved in plasma. The solubility of oxygen in plasma is low, and in normobaric conditions the greatest proportion of oxygen by far is transported bound to Hb.
Hb is normally 97 percent saturated when breathing air at 1 atmosphere of pressure, so there is little potential for increasing oxygen transport on Hb by increasing the partial pressure of oxygen. In contrast, dissolved oxygen increases linearly with the partial pressure of oxygen, although it is only in hyperbaric conditions with a high fraction of inspired oxygen that the dissolved fraction becomes significant.
At 3 atmospheres and breathing air, there is still only a relatively small amount of dissolved oxygen. Breathing 100 percent oxygen at 3 atmospheres, however, results in a dissolved fraction sufficient to meet the body’s needs at rest in the absence of Hb, hence the value of receiving hyperbaric oxygen in conditions in which oxygen delivery is compromised (such as anemia and carbon-monoxide poisoning).
Carbon dioxide: Unlike oxygen, which is supplied at increasing partial pressures at depth, the number of molecules of carbon dioxide that are produced remains constant for a given workload, irrespective of depth. Transport of the carbon-dioxide load from tissues to lungs, however, may be less efficient in the hyperbaric environment, where an increased partial pressure of oxygen causes a fall in Hb in venous blood. Reduced Hb forms carbamino compounds with carbon dioxide and buffers the hydrogen ion resulting from the hydration of carbon dioxide in red blood cells. These are two of the quantitatively less important mechanisms of carbon-dioxide transport, however, and the significance of this disturbance is questionable.
Changes in Control of Respiration
Oxygen: Oxygen is transported in the blood either bound to hemoglobin (Hb) or dissolved in plasma. The solubility of oxygen in plasma is low, and in normobaric conditions the greatest proportion of oxygen by far is transported bound to Hb.
Hb is normally 97 percent saturated when breathing air at 1 atmosphere of pressure, so there is little potential for increasing oxygen transport on Hb by increasing the partial pressure of oxygen. In contrast, dissolved oxygen increases linearly with the partial pressure of oxygen, although it is only in hyperbaric conditions with a high fraction of inspired oxygen that the dissolved fraction becomes significant.
At 3 atmospheres and breathing air, there is still only a relatively small amount of dissolved oxygen. Breathing 100 percent oxygen at 3 atmospheres, however, results in a dissolved fraction sufficient to meet the body’s needs at rest in the absence of Hb, hence the value of receiving hyperbaric oxygen in conditions in which oxygen delivery is compromised (such as anemia and carbon-monoxide poisoning).
Carbon dioxide: Unlike oxygen, which is supplied at increasing partial pressures at depth, the number of molecules of carbon dioxide that are produced remains constant for a given workload, irrespective of depth. Transport of the carbon-dioxide load from tissues to lungs, however, may be less efficient in the hyperbaric environment, where an increased partial pressure of oxygen causes a fall in Hb in venous blood. Reduced Hb forms carbamino compounds with carbon dioxide and buffers the hydrogen ion resulting from the hydration of carbon dioxide in red blood cells. These are two of the quantitatively less important mechanisms of carbon-dioxide transport, however, and the significance of this disturbance is questionable.
Net Effects of Respiratory Alterations
Sustained work output by tissues is largely limited by their oxygen supply. In normal exercise, tissue oxygen supply is limited by cardiac output rather than ventilation or gas exchange. In a healthy person ventilation can be dramatically increased to 200 liters per minute or more, and a rapid transit of blood through alveolar capillaries (normally about 0.35 seconds) in high-output situations does not prevent equilibration of gases across the respiratory barrier. In addition, the ventilation/perfusion profile of the lung usually improves during exercise.

Underwater, even at the relatively modest depth of 100 feet commonly attained by sport divers, air density/airway resistance factors mediate a reduction in maximum voluntary ventilation to approximately half the surface value. This reduction in ventilatory capacity, the concomitant increase in the work and oxygen cost of breathing, the increase in underventilated and/or overperfused lung units and dead-space effects determine that underwater work may be ventilation-limited rather than perfusion-limited. It can be readily appreciated that a diver at a modest depth swimming into a 1-knot current (oxygen consumption for fin swimming at 1 knot is roughly 2 liters per minute), wearing ill-fitting equipment, using a poorly maintained regulator and being subject to the above physiologic compromise might fail to sustain the required work to make progress.
Another important consequence of these respiratory alterations is the diver’s predisposition to retain carbon dioxide. Factors contributing to this situation include increased work of breathing (which increases carbon-dioxide production and limits ventilation), decreased respiratory drive, decreased carbon-dioxide sensitivity in some divers, skip breathing and dead-space effects. The consequences of hypercapnia in divers include unpleasant and dangerous symptoms such as dyspnea, headache, nausea and unconsciousness as well as potentiation of nitrogen narcosis, oxygen toxicity and decompression illness.
II. THE CARDIOVASCULAR SYSTEM
Changes in Blood Volume Distribution
When a diver is immersed, the hemodynamic effect of gravity is abolished, and there is a consequent redistribution of peripheral blood into the central circulation. This effect is enhanced in cold water when peripheral vasoconstriction further promotes this redistribution. The relative central hypervolemia increases the activity of stretch receptors in the walls of the great veins and right atrium, with receptors in the carotid sinus and aortic arch also involved if the blood shift is sufficient to increase mean arterial pressure. The increased stretch receptor activity mediates a decrease in production of antidiuretic hormone from the hypothalamus/posterior pituitary. This results in an increased permeability to water in renal distal tubule cells and, therefore, increased urinary loss of water. The net result is an undesirable tendency toward dehydration, which may be exacerbated by lack of adequate drinking water and/or seasickness.
Cardiac Effects
Immersion has been shown to increase cardiac output by up to 32 percent in thermoneutral water (approximately 91°F-94°F). The mechanism is an increase in venous return due to the centralization of blood volume. The increased preload, manifest as increased stretching of the heart muscle fibers during diastole, invokes the Frank-Starling mechanism in which the force of contraction is raised to cope with the extra volume. Stroke volume is therefore increased. In colder water the increase in cardiac output is less due to a concomitant bradycardia (decreased heart rate).

A bradycardia is associated with immersion. The “mammalian dive reflex” provoked by cold water contacting the face includes a bradycardia. In predisposed individuals the vagal outflow can be intense enough to produce asystole (cessation of heart beat) or arrhythmias (abnormal heart rhythms), which may lead to unexplained drowning after leaping into cold water. A bradycardia is produced even in a dry chamber at elevated ambient pressure, however, and researchers have sought other explanations for the immersion bradycardia in divers.
It has been demonstrated that an increase in the partial pressure of oxygen and the narcotic effect of inert gasses can produce a fall in heart rate on average of 10 beats per minute in divers, independent of the dive reflex. The degree of bradycardia is increased in colder water, and concomitantly so is the risk of arrhythmias in predisposed individuals. The role of these factors in diving fatalities, however, is largely unknown.
Another mechanism of bradycardia of questionable significance in divers, but one that is often mentioned in the diver training literature, is the carotid sinus reflex. There is a theoretical possibility that a wetsuit hood that fits too tightly around the neck may stimulate a carotid sinus reflex and therefore bradycardia.
Views differ on the net effect of these mechanisms on mean arterial blood pressure. It is likely that blood pressure remains within healthy parameters in the hyperbaric environment.
In conclusion, a better understanding of the physiological processes involved in breathing underwater can lead to enhanced comfort and safety during dives as well as an improved ability to assist a diver in trouble.
Reference
Edmonds C, Lowry C, Pennefather J, Walker R, eds. Diving and Subaquatic Medicine, 4th edition. London: Hodder Arnold, 2002.
© Alert Diver — Q3 Summer 2016