Q: My husband and I are planning a trip this fall to Papua New Guinea, where we expect to enjoy several days of diving and a couple days of trekking through some heavily forested areas. We’ve been reading about recommendations for anti-malaria medications. Are these drugs really necessary?
A: Malaria is indeed endemic to Papua New Guinea, and the serious health risk posed by this disease cannot be overstated. Anti-malarial drugs, as prescribed by your physician, are a vital part of an overall plan to prevent infection whenever you are traveling in a known malarial zone.
The malaria parasite, a protozoan of the genus Plasmodium, is transmitted to humans by the bite of an infected Anopheles mosquito, usually between dusk and dawn. After an incubation period of 13-17 days, symptoms develop; they are characterized by an abrupt onset of chills, shivering, sweating and high fevers. Fevers may occur daily until settling into a cyclical pattern.
Remember the ABCDs of malaria prevention:

- Awareness (Understand the risk and severity of malaria.)
- Bite prevention (Reduce the risk of malaria through appropriate precautions.)
- Chemoprophylaxis (Work with your doctor to select the most appropriate drug, and complete the course of pills.)
- Diagnosis (Understand the signs and symptoms of malaria; should they occur, seek medical help immediately.)
Discuss your travel plans with your physician well before departure. Many anti-malarial drugs require that you begin taking them days, sometimes weeks, before departure. The drug options will vary according to the strain of malaria found in your destination. All the drugs used for malaria prophylaxis are considered safe and are generally well tolerated, but side effects and toxic reactions can occur — some of them serious. Nonetheless, the risk of malaria may warrant tolerating temporary side effects. If a diver is unable to take a preventive medication because of side effects, the trip should be canceled or the medication changed to ensure coverage; the risk of contracting malaria is simply too great.
There have been no studies conducted on malaria medication use while diving. In the absence of scientific data, we recommend caution and stability on the drug before attempting any dive. Divers should also note that the potential side effects of the anti-malarial drug mefloquine (sometimes sold under the brand name Lariam) may mimic symptoms of decompression illness.
While drug prophylaxis is vital, it’s even more important to prevent the insect bites that transmit the disease. The use of prescribed medication without complementary bite prevention through the use of clothing and insect repellents is inadequate; it’s like driving without seatbelts while thinking your airbags will suffice in the event of an auto accident.
To avoid mosquito bites, stay in well-screened areas while indoors, and wear clothes that cover most of the body when outdoors. Use mosquito nets for sleeping, and when you go outside use insect repellent containing at least 30 percent DEET. Stronger concentrations can be used with caution. Permethrin, a synthetic chemical available in over-the-counter strengths of 1 percent and 5 percent, is also commonly used to treat clothing and mosquito nets. Use these with care and according to manufacturers’ instructions.
Even with aggressive preventive means, it is still possible to contract malaria. Symptoms may develop well after the trip is over, so follow your physician’s advice, and finish the complete course of anti-malarial drugs prescribed. If flu-like symptoms (any illness with chills, fever and headache) develop during a trip within a malaria-endemic area or within several months after the last exposure, seek qualified medical attention immediately.
— Daniel A. Nord, BFA, EMT-P, CHT, director of DAN Medical Services
Q: I am interested in becoming a certified diver, and I take Paxil for depression. Is there anything I need to know about diving while taking this drug?
A: The primary consideration when diving while taking any particular drug should always be the medical condition for which the drug is taken. You and your doctor should discuss any aspects of your depression that might cause impairment while diving. If you have uncontrolled symptoms like anxiety, suicidal thoughts or manic tendencies that could impair your awareness or judgment, diving is not advised. DAN recommends using new medications for at least 30 days before diving so you experience any side effects on land. This practice helps to ensure familiarity with the drug’s effects and minimizes the risk of new side effects occurring underwater.
Paxil falls into a class of drugs called selective serotonin reuptake inhibitors (SSRIs), which are known to be used by divers, so it’s unlikely your doctor would recommend against diving based solely on the fact that you take this medication. However, some common side effects of Paxil could be problematic for divers; they include dizziness, nervousness and headache. You should also know that it is theoretically possible for side effects to intensify while diving.
Bottom line: Get the approval of your mental health professional or physician before beginning your certification course, and if he or she has any questions about whether you should be diving, encourage your physician to give us a call on the DAN® Medical Information Line, +1-919-684-2948, ext. 222.
— Brian Harper, EMT, DMT, DAN medical information specialist
Q: My ophthalmologist has scheduled me for cataract surgery next week. The surgery will include lens implants. I have scheduled a dive vacation three months from now and am curious to know if it is OK to dive after lens implant surgery. My ophthalmologist doesn’t think it will be a problem, but he admits he is not trained in dive medicine.
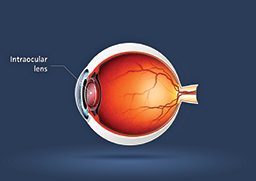
A: Intraocular lens implantation is a commonly performed surgical procedure for cataracts and refractive surgery. It generally involves replacing the natural crystalline lens of your eye with a flexible plastic lens; the procedure is usually done on an outpatient basis under local anesthesia. It involves the placement of the lens through a small incision on the surface of the eye; the incision is then sealed without a suture. Patients generally achieve full recovery within two to three weeks, but they should consult their physicians before participating in any strenuous physical exercise and activities that may increase blood pressure. Complications are rare but can involve infection, inflammation, loosening of the lens and visual disturbances (e.g., nighttime halos).
Scuba diving after lens implant surgery should not be a problem provided you allow enough time for the incision to heal. The healthy eye is filled with a non-compressible fluid (aqueous and vitreous humors), so the changing pressures experienced during a dive are evenly distributed and pose no particular threat.
There have been no controlled studies that specifically address the wait time required before returning to diving after such a procedure, so your best course of action is to play it safe. Wait a minimum of two months and then consult your treating physician to review your recovery before returning to diving.
— John U. Lee, MSDT, CHT, DAN medical information specialist
Q: I think I have a middle-ear squeeze from yesterday’s dive, and we are due to fly home in a couple of days. I have stopped diving because of the symptoms. My ear feels clogged, and I don’t feel like I can equalize. Am I going to be safe to fly?
A: You were wise to stop diving. Continuing to dive with a pre-existing ear squeeze (barotrauma) can aggravate the symptoms and even cause permanent injury. If you experience serious or worsening symptoms such as balance problems, vertigo, intense pain, nausea, hearing loss (not just muffled hearing) or persistent ringing or roaring in the ear, seek prompt medical attention from a local physician before flying. Fortunately, the symptoms you describe fall into the less-serious category. A clogged sensation in the ears, the sensation of “water in the ears,” muffled hearing and a clicking or bubbling noise are less likely to be a problem for a flight planned two days in the future, but these symptoms may still warrant evaluation and treatment from a local doctor.
Whether flying or diving, you need to be able to equalize the pressure in your ears. The pressure changes inside a commercial aircraft cabin are far less dramatic than those encountered while diving and are typically not enough to cause further injury in the case of mild, properly treated barotrauma, but an inability to equalize will create significant discomfort. To reduce symptoms and improve equalization, a doctor will usually recommend over-the-counter medications such as decongestants and/or anti-inflammatories. More serious symptoms may require prescription medications.
— Marty McCafferty, EMT-P, DMT-A, DAN medical information specialist
© Alert Diver — Q2 Spring 2010